A new high-cost specialty drug comes to market nearly every week. These drugs contribute to the exponential rise in pharmacy costs currently impacting employers. In fact, specialty drug costs have surpassed non-specialty drugs as a percentage of overall pharmacy costs for most employers.
Given this environment, WTW leverages our expertise and history in pharmacy benefits to identify potential cost-saving opportunities for our employer clients. We transformed pharmacy benefit delivery for employers by creating the Rx Collaborative (RxC) group purchasing coalition over 15 years ago. Since then, the RxC has grown to provide a pharmacy solution to more than 650 employer groups, who collectively saved more than a billion dollars in drug spend.
While the RxC’s group purchasing power has made an important difference in drug costs, we continue to look for additional solutions to reduce the pharmacy burden. In particular, we see a clear need to evaluate the management of specialty and non-specialty pharmacy benefits to create a tangible advantage for both the employer and member. This would potentially utilize separate vendors to manage and administer pre-defined portions of the pharmacy benefit.
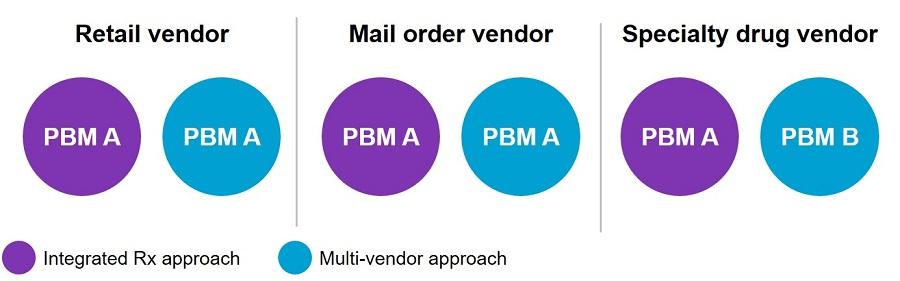
To fully vet a multi-vendor approach, we issued a focused request for proposal (RFP) to analyze the impact on the member experience, clinical performance and overall financial value. Despite a significant amount of interest in the marketplace for this new strategy, a limited number of vendors responded to the RFP. The lack of participation demonstrates that most PBMs are currently interested only in providing a standard integrated PBM offer rather than a multi-vendor/specialty carve-out offer.
After a thorough review of the participating vendor responses, WTW confirmed that there is no compelling financial or qualitative reason to pursue a full carve-out of specialty drugs from the PBM at this time. In fact, a shift to this type of new model could result in a significant financial loss to employers. Our analysis revealed that the potential cost to separate specialty from non-specialty pharmacy management was more than 10% higher than the current pricing structure. Of critical importance, only a handful of specialty pharmacy vendors were willing to provide meaningful financial guarantees. Without guarantees, employers would face significant financial risks on more than half their overall drug spend.
In essence, our analysis of new disruptors in the marketplace shows that these vendors have some interesting and unique approaches to managing specialty drug utilization but are not yet ready to offer a fully viable replacement to the current PBM model. We will continue to test the value of such a solution, since enhancements to the financial, clinical and member experience are still very much needed. Yet, some bright signs are on the horizon as some vendors are now willing to carve out specific specialty therapy classes (hemophilia, fertility, etc.) and others are close to adding new capabilities such as pharmacogenomics (the study of how a person's unique genetic makeup (genome) influences his or her response to medications).
Until further advances are made, employers of 1,000 employees or more can look to proven market-leading alternatives ─ like our RxC ─ that provide value today. RxC employers experience immediate savings as high as 20% of total drug spend through aggressive pricing and clinical management ─ and gain access to the expertise of more than 100 WTW colleagues dedicated to pharmacy consulting.
The findings from our RFP support our current RxC model, but we will continue to investigate additional solutions. As part of that effort, we will expand relationships with vendors and partners and push them to generate meaningful cost reductions for our employer clients’ pharmacy benefits programs.
While there are several ways to tackle rising specialty drug costs, we recommend focusing on three key areas:
The WTW pharmacy community is available to provide support in the management of pharmacy benefits including specialty, to assist employers in controlling costs and maximizing value for their employees.